
A senior health chief has vowed to work to rebuild trust following a damning report into the response to complaints raised about a Belfast neurologist.
The Independent Neurology Inquiry found systems and processes around patient safety failed, and opportunities to intervene in the practice of Dr Michael Watt were not taken by the Belfast Health Trust, as early as 2006.
Failures were not confined to the trust, with the Ulster Independent Clinic, where Dr Watt had a substantial private practice, criticised for the “failure to disclose significant complaints”.
The report said that information was “essentially retained in silos” and communication between different organisations was “poor and inadequate”.
The report makes 76 recommendations to the Department of Health, healthcare organisations, General Medical Council and the independent sector.
Reacting to the report, former patients said they were failed, and urged accountability, “not just corporate accountability”.
Dr Cathy Jack, chief executive of the Belfast Health Trust, apologised to the former patients, saying the trust let them down.
She said she would not be resigning, adding she did not believe this “incredibly difficult time” for the health service and trust would be improved if leaders “abandon their posts”.
“I have important work to do in very difficult circumstances in order to build safer and better services for patients, service users and staff, and I intend to get on with doing it,” she said.
Health Minister Robin Swann has issued a statement on the Independent Neurology Inquiry Report.
Read ➡️https://t.co/ClP1F63RJq pic.twitter.com/UWS9FSjo2B
— Department of Health (@healthdpt) June 21, 2022
Dr Jack said public confidence in the Belfast Trust and the wider medical profession is being tested because one doctor let down many of his patients, and the trust missed opportunities to have detected this earlier.
“However, that one doctor does not reflect the entirety of the 21,000 staff in the Belfast Trust today,” she said.
“It is essential that where trust has been lost, that it is rebuilt.
“The vast majority of doctors, both working in the Belfast Trust and elsewhere, provide safe and high quality care for their patients.
“They provide that care with integrity and compassion. They do so because they put their patients first.“
Peter McNaney, chairman of the Belfast Trust, said the trust is determined to do everything it can to learn from the experience and the recommendations.
Trust statement in response to the Independent Neurology Inquiry report released today: https://t.co/joS14zAlyN
The full report is available at: https://t.co/YlzXf9MuCA pic.twitter.com/tYsiFtz6Ft
— Belfast Trust (@BelfastTrust) June 21, 2022
He said the trust has already taken a number of steps to address some of the major concerns identified by the inquiry.
Health Minister Robin Swann also apologised and described the report as “difficult reading”.
He said the report was “extensive and detailed”, and pledged to ensure it is “given the careful and measured consideration it deserves”.
“I am determined that this analysis should happen as quickly as possible,” he said.
Charlie Massey, chief executive of the General Medical Council, said it acknowledges that during its investigations it “could and should have done more to act on clinical concerns sooner and to share information more effectively with other organisations”.
“We are sorry that we did not,” he said, adding they will “carefully consider” the recommendations.
Dr Watt was at the centre of Northern Ireland’s largest recall of patients, which began in 2018, after concerns were raised about his clinical work.
More than 4,000 of his former patients attended recall appointments.
Almost a fifth of patients who attended recall appointments were found to have received an “insecure diagnosis”.
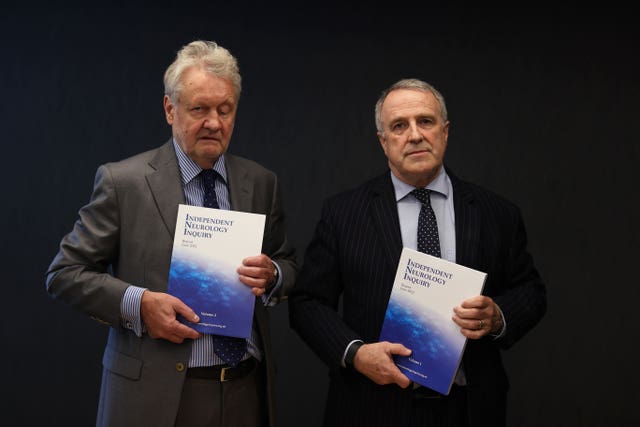
The inquiry, led by Brett Lockhart QC, concluded that the trust could and should have intervened earlier but failed to do so.
The report also found that while not every step taken after November 2016 was correct, the inquiry panel believes the Belfast Trust got key decisions right after that date.
Those included the partial restriction of Dr Watt in December 2016, the commissioning of a report into his practice by the Royal College of Physicians, the full restriction of his practice in July 2017 and the decision to initiate a large-scale patient recall in May 2018.
Danielle O’Neill, a former patient of Dr Michael Watt, says she and the other patients were failed. pic.twitter.com/WmOq1LvgkN
— Rebecca Black (@RBlackPA) June 21, 2022
“Patients will, however, rightly point to the many years when problems that emerged with Dr Watt were not addressed, opportunities were missed and such inaction was to the significant detriment of patients,” the report added.
Mr Lockhart said the inquiry panel concluded that the Belfast Trust “could and should have intervened earlier but failed to do so over many years”.
He said: “The onus is now on everyone involved in the delivery of healthcare, from the political representatives to the Department of Health and the Health Trusts, from the regulator to the independent sector, to ensure the recommendations of this report are properly considered and implemented.
“The goal is a healthcare system which makes patient safety its paramount concern whatever the question being asked, or the issue determined. Patients who have waited for so many years deserve nothing less.”
Danielle O’Neill, a former patient of Dr Michael Watt, was among those who attended the publication of the report.
“Michael Watt failed us, the Belfast Trust failed us, the Department of Health failed us, the GMC failed every single patient caught up in this scandal,” she said.
“They should all do the honourable thing, hang their heads in shame and resign.”
Dr Watt was granted voluntary erasure by the Medical Practitioners Tribunal Service before the allegations against him were heard at a hearing.
This means he can no longer practise medicine in the UK.


Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here